Valves
Main article: Heart valves
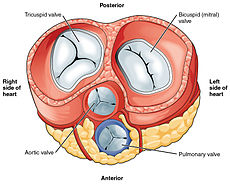
All four heart valves lie along the same plane. The valves ensure unidirectional blood flow through the heart and prevent backflow. Between the right atrium and the right ventricle is the tricuspid valve. This consists of three cusps (flaps or leaflets), made of endocardium reinforced with additional connective tissue. Each of the three valve-cusps is attached to several strands of connective tissue, thechordae tendineae (tendinous cords), sometimes referred to as the heart strings. They are composed of approximately 80 percent collagenous fibers with the remainder consisting of elastic fibers and endothelium. They connect each of the cusps to apapillary muscle that extends from the lower ventricular surface. These muscles control the opening and closing of the valves. The three papillary muscles in the right ventricle are called the anterior, posterior, and septal muscles, which correspond to the three positions of the valve cusps.
Between the left atrium and left ventricle is the mitral valve, also known as the bicuspid valve due to its having two cusps, an anterior and a posterior medial cusp. These cusps are also attached via chordae tendinae to two papillary muscles projecting from the ventricular wall.
The tricuspid and the mitral valves are the atrioventricular valves. During the relaxation phase of the cardiac cycle, the papillary muscles are also relaxed and the tension on the chordae tendineae is slight. However, as the ventricle contracts, so do the papillary muscles. This creates tension on the chordae tendineae, helping to hold the cusps of the atrioventricular valves in place and preventing them from being blown back into the atria.[7]
The semilunar pulmonary valve is located at the base of the pulmonary artery. This has three cusps which are not attached to any papillary muscles. When the ventricle relaxes blood flows back into the ventricle from the artery and this flow of blood fills the pocket-like valve, pressing against the cusps which close to seal the valve. The semilunar aortic valve is at the base of the aorta and also is not attached to papillary muscles. This too has three cusps which close with the pressure of the blood flowing back from the aorta.[7]
Right heart
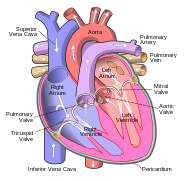
The two major systemic veins, the superior and inferior venae cavae, and the collection of veins that make up the coronary sinus which drains the myocardium, empty into the right atrium. The superior vena cava drains blood from above thediaphragm and empties into the upper back part of the right atrium. The inferior vena cava drains the blood from below the diaphragm and empties into the back part of the atrium below the opening for the superior vena cava. Immediately above and to the middle of the opening of the inferior vena cava is the opening of the thin-walled coronary sinus.[7]
In the wall of the right atrium is an oval-shaped depression known as the fossa ovalis, which is a remnant of an opening in the fetal heart known as the foramen ovale. The foramen ovale allowed blood in the fetal heart to pass directly from the right atrium to the left atrium, allowing some blood to bypass the pulmonary circuit. Within seconds after birth, a flap of tissue known as the septum primum that previously acted as a valve closes the foramen ovale and establishes the typical cardiac circulation pattern.[7] Most of the internal surface of the right atrium is smooth, the depression of the fossa ovalis is medial, and the anterior surface has prominent ridges of pectinate muscles, which are also present in the right atrial appendage.[7]
The atria receive venous blood on a nearly continuous basis, preventing venous flow from stopping while the ventricles are contracting. While most ventricular filling occurs while the atria are relaxed, they do demonstrate a contractile phase when they actively pump blood into the ventricles just prior to ventricular contraction. The right atrium is connected to the right ventricle by the tricuspid valve.[7]
When the myocardium of the ventricle contracts, pressure within the ventricular chamber rises. Blood, like any fluid, flows from higher pressure to lower pressure areas, in this case, toward the pulmonary artery and the atrium. To prevent any potential backflow, the papillary muscles also contract, generating tension on the chordae tendineae. This prevents the flaps of the valves from being forced into the atria and regurgitation of the blood back into the atria during ventricular contraction.[7]
The walls of the right ventricle are lined with trabeculae carneae, ridges of cardiac muscle covered by endocardium. In addition to these muscular ridges, a band of cardiac muscle, also covered by endocardium, known as the moderator bandreinforces the thin walls of the right ventricle and plays a crucial role in cardiac conduction. It arises from the lower part of the interventricular septum and crosses the interior space of the right ventricle to connect with the inferior papillary muscle.[7]
When the right ventricle contracts, it ejects blood into the pulmonary artery, which branches into the left and right pulmonary arteries that carry it to each lung. The upper surface of the right ventricle begins to taper as it approaches the pulmonary artery. At the base of the pulmonary artery is the pulmonary semilunar valve that prevents backflow from the pulmonary artery.[7]
Left heart
After gas exchange in the pulmonary capillaries, blood high in oxygen returns to the left atrium via one of the fourpulmonary veins. Only the left atrial appendage contains pectinate muscles. Blood flows nearly continuously from the pulmonary veins back into the atrium, which acts as the receiving chamber, and from here through an opening into the left ventricle. Most blood flows passively into the heart while both the atria and ventricles are relaxed, but toward the end of theventricular relaxation period, the left atrium will contract, pumping blood into the ventricle. This atrial contraction accounts for approximately 20 percent of ventricular filling. The left atrium is connected to the left ventricle by the mitral valve.[7]
Although both sides of the heart will pump the same amount of blood, the muscular layer is much thicker in the left ventricle compared to the right, due to the greater force needed here. Like the right ventricle, the left also has trabeculae carneae, but there is no moderator band. The left ventricle is the major pumping chamber for the systemic circuit; it ejects blood into the aorta through the aortic semilunar valve.[7]


0 comments:
Post a Comment